What Is Heart Failure?
Heart failure is a condition that occurs when the heart is unable to pump blood around the body as effectively as it should. Despite its name, it doesn’t mean the heart has stopped working. Instead, it means the heart needs support to function properly. At WKCP, we often see patients who are initially anxious about the term “heart failure”, but with the right understanding and management, many go on to live full and active lives. This guide explains what heart failure is, what causes it, how it’s diagnosed, and the treatments available.
Understanding Heart Failure
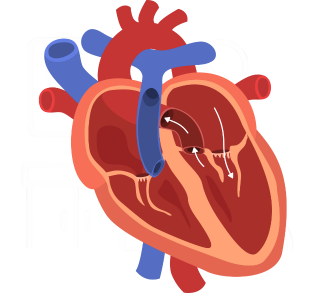
Your heart acts as a pump, sending blood and oxygen to every part of your body. When it becomes weaker or stiffer, it cannot deliver enough blood to meet the body’s needs. This can cause fatigue, breathlessness, and swelling, particularly in the legs and ankles.
There are two main types of heart failure:
- Left-sided heart failure: The left ventricle (the main pumping chamber) struggles to push blood around the body efficiently.
- Right-sided heart failure: The right side of the heart cannot pump blood effectively to the lungs, leading to fluid build-up.
Heart failure can develop suddenly (acute) or gradually over time (chronic).
What Causes Heart Failure?
Heart failure is usually the result of another underlying condition that has weakened or damaged the heart. The most common causes include:
- Coronary artery disease (CAD): Blocked or narrowed arteries reduce the oxygen supply to the heart muscle.
- High blood pressure: Puts extra strain on the heart, causing it to work harder.
- Heart attack: Can damage the heart muscle, leaving it weaker.
- Heart valve disease: Faulty valves make it harder for blood to flow smoothly.
- Cardiomyopathy: A disease that changes the heart’s structure or function.
- Arrhythmias: Irregular heart rhythms that affect how efficiently the heart pumps.
- Excessive alcohol or drug use: Can damage the heart muscle over time.
At our clinic, we often assess patients with multiple risk factors, helping to identify and manage each underlying cause to improve long-term heart health.
Symptoms of Heart Failure
The symptoms of heart failure can vary in severity, but the most common include:
- Shortness of breath during activity or when lying down
- Fatigue or feeling unusually tired
- Swelling in the ankles, legs, or abdomen
- Rapid or irregular heartbeat
- Sudden weight gain from fluid build-up
- Persistent coughing or wheezing
- Reduced ability to exercise or be active
Symptoms often develop slowly, so it’s easy to mistake them for general ageing or lack of fitness. However, early diagnosis makes a big difference in how well heart failure can be managed. If you notice any of these symptoms, it’s important to speak to your GP or a cardiologist.
How Heart Failure Is Diagnosed
Diagnosing heart failure involves a combination of medical history, physical examination, and diagnostic testing.
Common tests include:
- Electrocardiogram (ECG): Records the electrical activity of your heart to detect irregular rhythms or damage.
- Echocardiogram: Uses ultrasound to show how well your heart chambers and valves are working.
- Chest X-ray: Helps identify fluid around the lungs or an enlarged heart.
- Blood tests (BNP or NT-proBNP): Detect markers that indicate heart strain.
- Cardiac MRI or CT scan: Provides detailed images to assess structure and function.
These tests allow cardiologists to determine how efficiently your heart is pumping and what may be causing the problem. For more on these tests, visit the our Glossary page.
How Heart Failure Is Treated
While heart failure cannot always be cured, it can usually be managed effectively. Treatment aims to relieve symptoms, improve quality of life, and prevent the condition from worsening.
1. Lifestyle Adjustments
Making small but consistent changes to your daily habits can have a big impact. This includes:
- Eating a heart-healthy diet low in salt and saturated fats
- Staying active with gentle, regular exercise (as advised by your doctor)
- Reducing alcohol intake and stopping smoking
- Monitoring your weight and fluid levels daily
- Managing stress and ensuring adequate rest
2. Medication
Several types of medication are used to help manage, including:
- ACE inhibitors or ARBs: Help relax blood vessels and lower blood pressure.
- Beta-blockers: Reduce strain on the heart and control heart rate.
- Diuretics: Help remove excess fluid from the body.
- Mineralocorticoid receptor antagonists (MRAs): Reduce fluid retention and improve survival.
- ARNIs (Angiotensin receptor-neprilysin inhibitors): Newer drugs that improve heart function in some patients.
Your cardiologist will review your condition and prescribe a combination of medicines suited to your needs.
3. Devices and Surgical Options
In some cases, devices may be used to help the heart work more efficiently:
- Pacemakers: Help regulate slow heart rhythms.
- Implantable cardioverter-defibrillators (ICDs): Detect and correct dangerous arrhythmias.
- Cardiac resynchronisation therapy (CRT): Helps both sides of the heart beat in sync.
- Surgery: In severe cases, procedures to repair valves or bypass blocked arteries may be recommended.
These treatments can greatly improve both life expectancy and daily comfort.
Living with Heart Failure
Being diagnosed with heart failure can feel daunting, but with careful management, many people continue to live active, fulfilling lives. Regular follow-up appointments are vital, as your cardiologist can adjust your treatment if symptoms change.
At WKCP, we work closely with patients to monitor progress and provide practical advice on managing lifestyle changes. Our aim is always to empower patients to take control of their heart health.
Support from family and friends also makes a big difference. Many people find that sharing concerns or joining heart support groups helps them stay motivated and positive. For daily management advice, the NHS Heart Failure Guide offers clear, practical information.
Preventing Heart Failure
Prevention starts with protecting your heart early. Keeping blood pressure, cholesterol, and blood sugar under control reduces the risk of developing heart failure later in life. Regular exercise, a balanced diet, and not smoking all play key roles in maintaining a healthy heart.
If you already have conditions such as coronary artery disease, diabetes, or high blood pressure, following your treatment plan closely and attending regular check-ups helps prevent progression massively.
Conclusion
It may sound alarming, but with early diagnosis, effective treatment, and the right lifestyle choices, it can be successfully managed. Understanding the symptoms and knowing when to seek help are the first steps towards better heart health.
We provide expert assessment, diagnosis, and ongoing management for people living with heart failure across Kent and East Sussex. Whether you are newly diagnosed or looking for long-term support, we can help you take control of your condition.
If you have symptoms such as breathlessness, swelling, or fatigue, you can contact us here to arrange a consultation and discuss your options for diagnosis and treatment. For more information about heart failure and its management, visit the British Heart Foundation or the NHS website.

